NEGATIVE PRESSURE WOUND THERAPY (NPWT)
NEGATIVE PRESSURE WOUND THERAPY (NPWT)
Introduction
Negative Pressure Wound Therapy (NPWT) is also known as topical NPWT, Vacuum sealing technique, sealed surface wound suction, Vacuum Assisted Closure (VAC) or Vacuum pack technique. This essentially involves the application of sub atmospheric pressure to a healing wound with the help of a porous dressing and a drain attached to a vacuum device and covered with a polyurethane film to make an air tight seal.
Since its introduction in the early 1990’s NPWT has become widely used in the management of complex wounds of various etiologies in in- patient as well as out- patient settings with significant success. It has now become gold standard of care for wounds like open abdominal wounds and dehisced sternal wounds following cardiac surgery. It is also now being applied in home care settings.
Principles and Mechanism of action of NPWT21
- Functional Principle
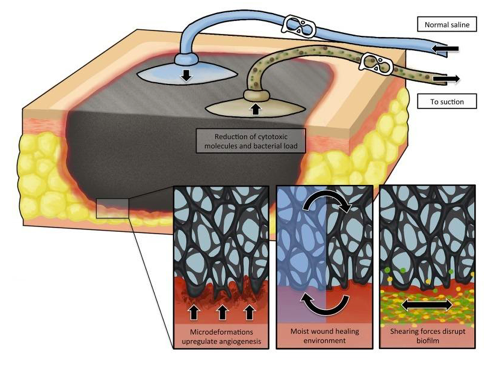
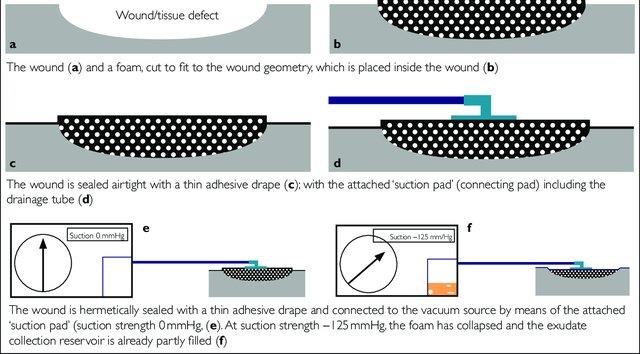
The principle of NPWT involves extending the usually narrowly defined suction effect of drainage across the entire area of the wound cavity or surface using an open-pore filler that has been fitted to the contours of the wound.
To prevent air from being sucked in from the external environment, the wound and the filler that rests inside or upon the wound are sealed with an airtight adhesive polyurethane drape that is permeable to water vapor, transparent, and bacteria proof. A connection pad is then applied over a small hole that has been made in the drape and connected to a vacuum source by means of a tube. 2
NPWT
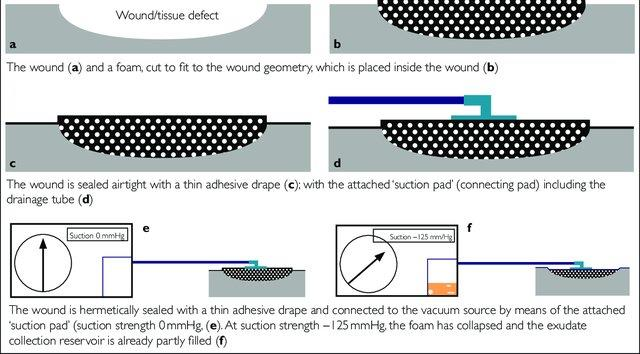
Figure 20: Functional Principle of NPWT
MECHANISM OF ACTION
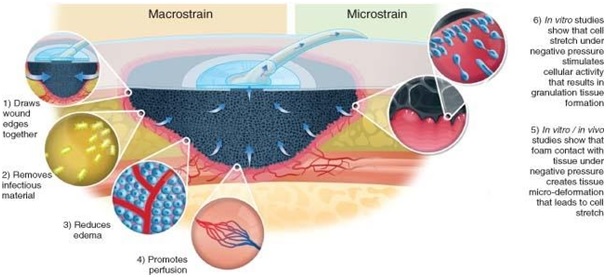
NPWT acts in different ways to promote wound healing. The wound is subject to suction pressure that is propagated through the wound filler to the wound bed. This suction drains exudate from the wound and creates a mechanical force in the wound edges that result in an altered tissue perfusion, angiogenesis and the formation of granulation tissue.
The following effects of NPWT on the wound healing and the affected tissue are considered to be the clinically significant mechanisms of action for this therapy.
- Creating A Moist Wound Environment
A moist environment is vital in wound healing as it facilitates the re- epithelialisation.
However, in an overly moist wound, exudate may cause infection and maceration, leading to damage to the wound edge. Removal of exudate is important to prevent the accumulation of necrotic tissue and slough that tend to continually accumulate in wounds 3
NPWT
and alter the biochemical and cellular environment. The accumulation of necrotic tissue or slough in a wound promotes bacterial colonisation and hinders repair of the wound. NPWT balances these effects, providing a moist wound environment while removing excess fluid.
- Removal Of Edema
Edema causes increased pressure on the wound tissue, which in turn compromises the microvascular blood flow, reducing the inflow of nutrients and oxygen. This reduces resistance to infections and inhibits healing.
NPWT causes compression of the tissue closest to the surface of the wound, which is believed to reduce interstitial edema
- Mechanical Effects On Wound Edges
NPWT mechanically stimulates the wound bed and produces a suction pressure on the wound edges that push onto the wound and contract it. These mechanical effects lead to tissue remodeling that may facilitate wound closure. It has also has been found that the wound tissue and the filler material interact on a microscopic level to micro deform the tissue. These mechanical deformations affect the cytoskeleton of the cells and initiate a cascade of biological reactions that may accelerate the formation of granulation tissue and subsequent wound healing by stimulating the expression of angiogenic growth factors and receptors, such as vascular endothelial growth factor (VEGF), VEGF receptors and the angiopoietin system receptors.
- Change in perfusion
NPWT has been shown to improve perfusion in a few studies. 4
NPWT
NPWT exerts compression on the tissue leading to an anti- edematous effect that might promote perfusion. It has also been speculated that the negative pressure causes a force in the tissue that opens up the capillaries, increasing flow.
- Change in bacterial count, bacterial clearance and immunological effects
NPWT offers a closed system for wound healing, as the adhesive drape provides a barrier against secondary infection from an external source and has been suggested to reduce the bacterial load in the wound. However it must be emphasized that the degree of bacterial colonisation is unrelated to the success or failure of NPWT. It is exceedingly important to perform proper debridement between dressing changes to mechanically remove the microorganisms.
- Molecular mechanisms in wound healing
It is hypothesized that the NPWT device induces the production of pro-angiogenic factors and promotes the formation of granulation tissue and healing.
NPWT is also associated with an up-regulation of basic fibroblast growth factor (bFGF) and extracellular signal-regulated kinase (ERK) 1/2 signaling, which may be involved in promoting the NPWT-mediated wound healing response.
NPWT also influences the local expression of pro inflammatory cytokines in tissue or fluid from acute infected soft-tissue. 5
NPWT
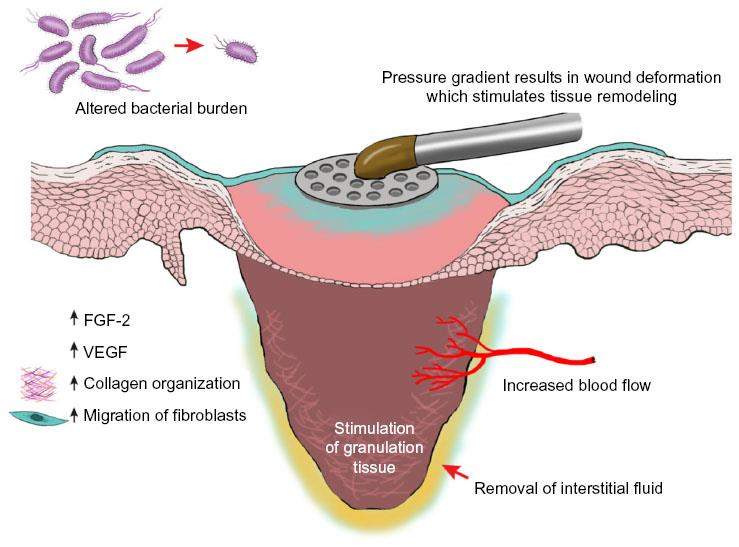
Figure 21: Proposed mechanism of action of NPWT
Advantages of NPWT
- Handling
o Hygienic wound closure—bacteria proof wound dressing for sealing the wound so no external bacteria can enter the wound and the patient’s own wound bacteria are not spread. This is particularly important in the event of contamination with problematic bacteria, as in patients with methicillin-resistant Staphylococcus aureus (MRSA)-infected wounds. Thus, it also reduces the risk of cross-infections and development of resistance within the hospital
o Transparent dressing permits continuous clinical monitoring of the surrounding skin through the film with which the wound has been sealed.
6
NPWT
o Odorless and hygienic dressing technique; constant seeping through the dressing onto the patient’s clothing and bedding can be avoided, reducing demands on the nursing staff
o Reduction in the number of required dressing changes (only necessary every two to three days), which reduces nursing time requirements, particularly in patients with exudating wounds.
o Compared with other forms of wound dressing, NPWT is easier to tailor and maintain in position. Almost every configuration of wound, including circumferential extremity wounds and wounds located in proximity to orthopedic fixation frames, can be managed with relative ease.
- Patient comfort
o Easy and early patient mobilization: Accelerated wound healing with NPWT significantly reduces the time to wound closure in diabetic patients, returning these patients to baseline more quickly and improving quality of life.
o Visually appealing dressing method due to clean, exudate-free dressing conditions, even during mobilisation.
Treatment Goals with NPWT22
- Provide a temporary wound cover
- Manage wound fluid and edema
- Accelerate patient mobility
- Improve pain management
- Prevent wound progression
- Increase dermal and wound perfusion
- Stimulate formation of granulation tissue
7
NPWT
- Enhance wound bed epithelialization
- Improve matrix material availability
- Reduce bacterial load
- Provide moist wound environment
- Influence expression of genes involved in wound healing
Treatment variables & Precautions
There are a number of different treatment variables related to NPWT that might affect wound healing. The level of negative pressure, the wound filler material (foam or gauze), the presence of wound contact layers, the pressure application mode (continuous, intermittent, or variable), or instillation of fluid may be chosen according to patient needs, disease, wound type and shape.
- Pressure level/ suction strength
Low pressures may be ineffective in draining the exudates while high pressures may be painful and have a negative effect on the microcirculation. The preferred range of pressure is between – 50 to -150 mm Hg. However there is no significant evidence to suggest an ideal clinical range and it is suggested that the negative pressure may be adjusted according to the circumstances. For example in patients with pain it can be appropriate to choose a suction setting less than −125 mmHg. Pressures as low as −40 mmHg may be used for the treatment of sensitive, poorly perfused tissue where there is a risk for ischemia, for example in the case of circumferential dressings, vascular disease, diabetic foot ulcers (DFUs) and thin skin transplants.
High output wounds will require high pressures for initial few days which may be lowered once the exudate lessens.
- Vacuum Source
8
NPWT
Traditional NPWT systems use an electrically powered pump to generate negative pressure at the wound bed. Recently portable devices that deliver NPWT without the use of an electrically powered pump have been introduced. These smaller light-weight devices are either battery powered or mechanically powered, and generate continuous sub-atmospheric pressure level to the wound bed between −75 and −125 mmHg. These devices allow the patient to be mobile and independent from hospital’s wall-suction on the ward and to be treated by NPWT in the home care setting.
Some battery-powered NPWT units use an electronically controlled feedback system that ensures the maintenance of the selected pressure level even in the presence of small air leaks, guaranteeing the effectiveness of NPWT. Additionally, audiovisual alarms alert the staff and the patients to large air leaks (loss of seal), blockage of the tubing and full canisters. These therapy units are designed to reduce complication and allow faults to be promptly recognized.
- Intermittent or continuous mode
NPWT can be applied in an intermittent or continuous or variable mode. The most common mode used currently is the continuous mode. Intermittent mode involves repeatedly switching on and off (usually 5 minutes on to 2 minutes off), while variable NPWT provides a smooth cycling between two different levels of negative pressure.
NPWT with intermittent suction has been shown to be of benefit for wound healing. This mode produces a mechanical stimulation of the wound bed (a massaging effect) and a greater circulatory stimuli, oxygenation and angiogenesis, and presumably a lower risk of occurrence of ischemic damage. Intermittent mode is however known to cause more pain.
New pressure cycles, without going to 0 mmHg suction, but only lowering the suction, to 50 % for example, should be able to maintain the highest degree of blood vessel 9
NPWT
formation and also a significant decrease in pain compared with the traditional intermittent group.
Under special wound conditions, when the wound involves structures such as the peritoneum, between toes, in tunneling injuries, in sternotomies, in the presence of high levels of exudate and when using NPWT on grafts or skin flaps, the continuous mode is the option of choice.
- Wound fillers
The choice of wound filler has been shown to have significant effect on wound healing. The commonly available material for this include foams and gauges with different pore sizes, stability etc.
The pressure distribution is similar for gauze and foam in dry wounds and the differences in performance are related to the structure of the material and its mechanical effects in the wound. The degrees of micro- and macrodeformation of the wound bed are similar after NPWT regardless of whether foam or gauze is used as wound filler. The increase in blood flow following NPWT is also similar with all wound fillers.
Wound contraction is more pronounced with foam than with gauze. Wound fluid retention is lower in foam, while more fluid is retained in the wound when using bacteria and fungus-binding mesh.
Thus NPWT may be tailored to the individual wound type to optimise the effects and minimize the complications by choosing different wound fillers. The choice of filler may be made with regard to the morphology of the wound, the wound characteristics, the patient feedback, possible infection and scar tissue formation.
o Wound morphology
Different wounds have different shapes and depths and thus require different fillers. 10
NPWT
Foam may fit better into a wound with a uniform shape, while gauze may be easier to apply in wounds that have an irregular shape, or with undermining edge since it can be better manipulated to the shape of the wounds. Different wound fillers can also be combined. Over a thin graft or a wound sleeve, the gauze will give a more appropriate cover. Foam may be advantageous for ‘bridging therapy’ since the foam compresses to a greater extent and thereby contracts the wound and speeds up the closure.
o Exuding wounds
In heavily exuding wounds, foam at a higher pressure (−120 mmHg) may be useful,
Since foam is less dense than gauze and a higher level of negative pressure drains the wound quicker.
o Wounds at risk of ischemia
In circumstances where there is a risk of ischemia, a lower pressure (−40 to −80 mmHg) and using gauze may be considered.
o Infected wounds
Various wound fillers designed for infected wounds include foam with silver, gauze that is impregnated with PHMB, gauze that is impregnated with silver, bacteria and fungus binding mesh.
Instillation techniques allow the irrigation of the wound with antiseptic solutions.
o Tendency to form excessive granulation tissue
Areas such as joints, where movement of the skin and the underlying tissue occur, may benefit from the use of gauze. Foam allows rapid growth of granulation tissue and may be a better choice in wounds where large amounts of granulation tissue is desirable, for example, postsurgical wounds such as sternotomy wounds.
- Wound contact layers
11
NPWT
Removal of foam used as fillers in NPWT can lead to pain and trauma. When the clinician anticipates such complications, a non- adherent wound contact layer such as paraffin or silicon may be placed over the wound bed beneath the wound filler. A wound contact layer also may be placed over vulnerable structures such as blood vessels or nerves. This wound contact layer may reduce the pain during dressing changes.
However keeping the quality of wound healing in mind, it is important to use wound contact layers only when there are structures to protect, in order not to slow healing.
- Protection of tissues and organs
NPWT can at times be the only option available to the treating clinician for managing highly infected and large wounds. However of late there have been reports of serious associated complications of NPWT.
The risk of right ventricular rupture and bypass graft bleeding following NPWT of mediastinitis is estimated to be between 4–7 % of all cases treated. Severe bleeding of large blood vessels such as the aorta has also been reported in several patients receiving NPWT. The incidence of NPWT-related bleeding in patients with exposed blood vessels or vascular grafts (such as femoral and femoral-popliteal grafts) in groin wounds were relevant in some studies. Severe bleeding has also been reported in patients receiving NPWT for burn wounds.
FDA has thus stated that NPWT is contraindicated in certain types of wounds: those with necrotic tissue with eschar, in non- enteric and unexplored fistulas, where malignancy is present, in wounds with exposed vasculature, anastomotic sites, exposed nerves, exposed organs and untreated osteomyelitis. 12
NPWT
It has been suggested that exposed sensitive structures need to be protected either through the interposition of autologous tissue (muscle flaps) or with heterologous material (dermal substitutes) or a number of wound contact layers.
- Pain treatment
Pain is a significant issue associated with NPWT and may affect patient adherence.
In patients that are neuropathic or paraplegic, where the pain is not of a significant nature, the filler can be used efficiently. In patients with low adherence, especially children and the elderly, and on painful lesions (such as pyoderma gangrenosum, burns, PUs and infected wounds), gauze, tends to be better tolerated.
Another option to reduce pain due to NPWT is to prepare the patient by infiltration of the wound filler with saline solution or local anaesthetics before dressing change.
Clinical Applications5
- Acute wounds
Acute wounds are often traumatic but can also be due to surgical debridement of infected or necrotic tissue. Wounds requiring extensive surgical debridement often present a wound dressing challenge due to anatomic location (eg, Fournier's gangrene), the size of the tissue defect, or the patient's body habitus.
- NPWT dressings can be applied immediately following operative debridement, which simplifies postoperative wound care. The ability of the foam and adhesive dressing to conform to almost any wound contour, shape, or size contributes to the success of NPWT in these complex wounds.
- NPWT can also be used in conjunction with skin grafts or flaps, which are frequently needed to cover tissue defects. NPWT has been used instead of traditional bolstering methods to provide skin graft fixation. The NPWT dressing distributes negative pressure
13
NPWT
uniformly over the surface of the fresh graft, immobilizing the graft with less chance of shearing leading to improved qualitative skin graft take and quantitative improvements in skin graft success.
- For acute open wounds, NPWT is associated with a reduced time to wound closure. NPWT has also been used to manage acute wounds resulting from lower extremity fasciotomy, degloving injury, open amputation, and complex traumatic wounds with exposed tendon, bone, or orthopedic hardware.
- NPWT may also have a particular role in the treatment of burn wounds.
- Chronic wounds
- NPWT may improve the healing of some types of chronic wounds/ulceration, such as diabetic foot ulcers, pressure ulcers, and open abdomen, provided that the wounds are well vascularized
- Post-sternotomy mediastinitis is an uncommon but devastating complication of cardiac surgery which may require the use of NPWT to manage the open wound while awaiting sternal closure.
- Prophylactic use
Evidence suggests that there may be a prophylactic role for NPWT in reducing the rates of surgical site infections.
Indications of NPWT
Trauma & Orthopedic Surgery
- Acute trauma & dermatofasciotomy wounds
NPWT is a tool in the treatment of traumatic wounds and high-risk incisions after surgery in
- contaminated acute wounds (open fractures, penetrating injuries) and wounds with tissue defects requiring a step wise procedure.
14
NPWT
- amputation stump resulting from a guillotine-like marginal zone amputation.
- management of motorcycle spoke heel injury
- perineal trauma-related wounds.
- Periprosthetic infections of the hip and knee joint
NPWT is a useful option in the management of early or delayed infections following implantation of an endoprosthesis.
- Osteomyelitis and surgical site infection
- Exposed tendon, bone and hardware
NPWT is the treatment of choice in such conditions where plastic surgery procedures cannot be used to provide immediate cover to exposed structures.
Acute burns and scalds
The management of burns with their associated high-fluid exudate following burn excision and skin grafting has always posed a challenge in burn wound care. The ideal dressing should protect the wound from physical damage and microorganisms; be comfortable and durable; allow high humidity at the wound; and be able to allow maximal activity for wound healing without retarding or inhibiting any stage of the process. NPWT fulfils all these criteria.
Plastic and reconstructive surgery
NPWT has produced a change of paradigms within the treatment algorithms in traditional reconstructive surgery.
NPWT may represent a valid alternative to immediate reconstruction in selected cases of acute complex traumas of the lower limb.
NPWT is a valid tool for reliable fixation of skin substitutes, such as tissue-engineered skin substitute and split skin grafts in all severe traumatised wounds and is associated with improved graft survival. 15
NPWT
Abdominal Surgery
NPWT is one of the techniques used for temporary abdominal closure (TAC) in laparotomies with packing, ACS or severe septic intra-abdominal complications.
Cardiovacscular Surgery
While NPWT is the method of choice for management of poststernotomy mediastinitis, its use is also being advocated over closed sternal incisions to reduce the incidence of deep sternal wound infection.
Vascular surgery
- Infected blood vessels and vascular grafts
For high-risk surgical patients with a fully exposed infected prosthetic vascular graft, NPWT along with aggressive debridement and antibiotic therapy is an effective alternative to current management strategies.
- Lymphocutaneous fistulas
NPWT can be used for the management of lymphocutaneous fistulae resulting from axillary and inguinal lymph node dissections as well as surgery of the infra-inguinal vessels.
Non-healing wounds
- Leg ulcers
Although NPWT has been used extensively in non healing leg ulcers, there is limited rigorous RCT evidence available concerning the clinical effectiveness of NPWT in the treatment of leg ulcers.
- Pressure ulcers
NPWT is increasingly being used to manage PUs, most likely due to its flexibility, which allows the caregivers to insert it into a more complex and articulated therapeutic strategy.
- Diabetic foot ulcer
16
NPWT
The rationale for adopting NPWT in DFUs is related to its capacity of removing exudate, protecting the wound from exposure to the environment, reducing odor and helping debridement.
Complications of NPWT5
NPWT is generally safe and well tolerated. Some of the important complications include bleeding, infection, pain, organ damage, and possibly death. Such complications are most likely to occur when NPWT is applied to patients whose wounds have devitalized tissue or exposed vital structures (eg, organs, blood vessels, vascular grafts).
- Bleeding
Bleeding is the most serious complication of NPWT and can occur in hospitals, long-term care facilities, and at home. Minor bleeding during dressing changes due to granulation tissue at the base of the wound is common and is best managed with firm pressure to the wound surface.
Severe hemorrhage can occur during removal of foam that has become adherent to the granulation tissue below, especially in patients who are anticoagulated, or in patients with exposed vessels or vascular grafts. In patients with severe bleeding, direct pressure should be applied and emergency services contacted. Surgery may be needed to control bleeding.
- Infection
Infection related to the use of NPWT is often due to prior wound infection that was inadequately controlled prior to initiating NPWT. When infection is suspected the NPWT dressing in discontinued, the wound irrigated and debrided, wound cultures obtained, and empiric antibiotics initiated.
- Enterocutaneous fistula
17
NPWT
Contraindications of NPWT21
- Risk of bleeding
NPWT should not be applied in wounds with manifest bleeding or a risk of bleeding, as suction could result in a significant blood loss.
Additionally the bleeding can clot the foam and therefore stop any function of the NPWT device.
- Exposed vessels and vascular prostheses
FDA has stated this as one of the contraindications for the use of NPWT.
- Necrotic wound bed
Necrotic tissue acts as a barrier to new tissue growth. The use of NPWT must therefore be preceded by radical debridement.
- Untreated osteomyelitis
Due to the deep extension of a potential osteomyelitic focus, simple surface treatment is unlikely to be successful. In this case, treatment must include the radical removal of the focus of infection.
- Malignant wounds
NEGATIVE PRESSURE WOUND THERAPY (NPWT)
Introduction
Negative Pressure Wound Therapy (NPWT) is also known as topical NPWT, Vacuum sealing technique, sealed surface wound suction, Vacuum Assisted Closure (VAC) or Vacuum pack technique. This essentially involves the application of sub atmospheric pressure to a healing wound with the help of a porous dressing and a drain attached to a vacuum device and covered with a polyurethane film to make an air tight seal.
Since its introduction in the early 1990’s NPWT has become widely used in the management of complex wounds of various etiologies in in- patient as well as out- patient settings with significant success. It has now become gold standard of care for wounds like open abdominal wounds and dehisced sternal wounds following cardiac surgery. It is also now being applied in home care settings.
Principles and Mechanism of action of NPWT21
- Functional Principle
The principle of NPWT involves extending the usually narrowly defined suction effect of drainage across the entire area of the wound cavity or surface using an open-pore filler that has been fitted to the contours of the wound.
To prevent air from being sucked in from the external environment, the wound and the filler that rests inside or upon the wound are sealed with an airtight adhesive polyurethane drape that is permeable to water vapor, transparent, and bacteria proof. A connection pad is then applied over a small hole that has been made in the drape and connected to a vacuum source by means of a tube. 2
NPWT
Figure 20: Functional Principle of NPWT
MECHANISM OF ACTION
NPWT acts in different ways to promote wound healing. The wound is subject to suction pressure that is propagated through the wound filler to the wound bed. This suction drains exudate from the wound and creates a mechanical force in the wound edges that result in an altered tissue perfusion, angiogenesis and the formation of granulation tissue.
The following effects of NPWT on the wound healing and the affected tissue are considered to be the clinically significant mechanisms of action for this therapy.
- Creating A Moist Wound Environment
A moist environment is vital in wound healing as it facilitates the re- epithelialisation.
However, in an overly moist wound, exudate may cause infection and maceration, leading to damage to the wound edge. Removal of exudate is important to prevent the accumulation of necrotic tissue and slough that tend to continually accumulate in wounds 3
NPWT
and alter the biochemical and cellular environment. The accumulation of necrotic tissue or slough in a wound promotes bacterial colonisation and hinders repair of the wound. NPWT balances these effects, providing a moist wound environment while removing excess fluid.
- Removal Of Edema
Edema causes increased pressure on the wound tissue, which in turn compromises the microvascular blood flow, reducing the inflow of nutrients and oxygen. This reduces resistance to infections and inhibits healing.
NPWT causes compression of the tissue closest to the surface of the wound, which is believed to reduce interstitial edema
- Mechanical Effects On Wound Edges
NPWT mechanically stimulates the wound bed and produces a suction pressure on the wound edges that push onto the wound and contract it. These mechanical effects lead to tissue remodeling that may facilitate wound closure. It has also has been found that the wound tissue and the filler material interact on a microscopic level to micro deform the tissue. These mechanical deformations affect the cytoskeleton of the cells and initiate a cascade of biological reactions that may accelerate the formation of granulation tissue and subsequent wound healing by stimulating the expression of angiogenic growth factors and receptors, such as vascular endothelial growth factor (VEGF), VEGF receptors and the angiopoietin system receptors.
- Change in perfusion
NPWT has been shown to improve perfusion in a few studies. 4
NPWT
NPWT exerts compression on the tissue leading to an anti- edematous effect that might promote perfusion. It has also been speculated that the negative pressure causes a force in the tissue that opens up the capillaries, increasing flow.
- Change in bacterial count, bacterial clearance and immunological effects
NPWT offers a closed system for wound healing, as the adhesive drape provides a barrier against secondary infection from an external source and has been suggested to reduce the bacterial load in the wound. However it must be emphasized that the degree of bacterial colonisation is unrelated to the success or failure of NPWT. It is exceedingly important to perform proper debridement between dressing changes to mechanically remove the microorganisms.
- Molecular mechanisms in wound healing
It is hypothesized that the NPWT device induces the production of pro-angiogenic factors and promotes the formation of granulation tissue and healing.
NPWT is also associated with an up-regulation of basic fibroblast growth factor (bFGF) and extracellular signal-regulated kinase (ERK) 1/2 signaling, which may be involved in promoting the NPWT-mediated wound healing response.
NPWT also influences the local expression of pro inflammatory cytokines in tissue or fluid from acute infected soft-tissue. 5
NPWT
Figure 21: Proposed mechanism of action of NPWT
Advantages of NPWT
- Handling
o Hygienic wound closure—bacteria proof wound dressing for sealing the wound so no external bacteria can enter the wound and the patient’s own wound bacteria are not spread. This is particularly important in the event of contamination with problematic bacteria, as in patients with methicillin-resistant Staphylococcus aureus (MRSA)-infected wounds. Thus, it also reduces the risk of cross-infections and development of resistance within the hospital
o Transparent dressing permits continuous clinical monitoring of the surrounding skin through the film with which the wound has been sealed.
6
NPWT
o Odorless and hygienic dressing technique; constant seeping through the dressing onto the patient’s clothing and bedding can be avoided, reducing demands on the nursing staff
o Reduction in the number of required dressing changes (only necessary every two to three days), which reduces nursing time requirements, particularly in patients with exudating wounds.
o Compared with other forms of wound dressing, NPWT is easier to tailor and maintain in position. Almost every configuration of wound, including circumferential extremity wounds and wounds located in proximity to orthopedic fixation frames, can be managed with relative ease.
- Patient comfort
o Easy and early patient mobilization: Accelerated wound healing with NPWT significantly reduces the time to wound closure in diabetic patients, returning these patients to baseline more quickly and improving quality of life.
o Visually appealing dressing method due to clean, exudate-free dressing conditions, even during mobilisation.
Treatment Goals with NPWT22
- Provide a temporary wound cover
- Manage wound fluid and edema
- Accelerate patient mobility
- Improve pain management
- Prevent wound progression
- Increase dermal and wound perfusion
- Stimulate formation of granulation tissue
7
NPWT
- Enhance wound bed epithelialization
- Improve matrix material availability
- Reduce bacterial load
- Provide moist wound environment
- Influence expression of genes involved in wound healing
Treatment variables & Precautions
There are a number of different treatment variables related to NPWT that might affect wound healing. The level of negative pressure, the wound filler material (foam or gauze), the presence of wound contact layers, the pressure application mode (continuous, intermittent, or variable), or instillation of fluid may be chosen according to patient needs, disease, wound type and shape.
- Pressure level/ suction strength
Low pressures may be ineffective in draining the exudates while high pressures may be painful and have a negative effect on the microcirculation. The preferred range of pressure is between – 50 to -150 mm Hg. However there is no significant evidence to suggest an ideal clinical range and it is suggested that the negative pressure may be adjusted according to the circumstances. For example in patients with pain it can be appropriate to choose a suction setting less than −125 mmHg. Pressures as low as −40 mmHg may be used for the treatment of sensitive, poorly perfused tissue where there is a risk for ischemia, for example in the case of circumferential dressings, vascular disease, diabetic foot ulcers (DFUs) and thin skin transplants.
High output wounds will require high pressures for initial few days which may be lowered once the exudate lessens.
- Vacuum Source
8
NPWT
Traditional NPWT systems use an electrically powered pump to generate negative pressure at the wound bed. Recently portable devices that deliver NPWT without the use of an electrically powered pump have been introduced. These smaller light-weight devices are either battery powered or mechanically powered, and generate continuous sub-atmospheric pressure level to the wound bed between −75 and −125 mmHg. These devices allow the patient to be mobile and independent from hospital’s wall-suction on the ward and to be treated by NPWT in the home care setting.
Some battery-powered NPWT units use an electronically controlled feedback system that ensures the maintenance of the selected pressure level even in the presence of small air leaks, guaranteeing the effectiveness of NPWT. Additionally, audiovisual alarms alert the staff and the patients to large air leaks (loss of seal), blockage of the tubing and full canisters. These therapy units are designed to reduce complication and allow faults to be promptly recognized.
- Intermittent or continuous mode
NPWT can be applied in an intermittent or continuous or variable mode. The most common mode used currently is the continuous mode. Intermittent mode involves repeatedly switching on and off (usually 5 minutes on to 2 minutes off), while variable NPWT provides a smooth cycling between two different levels of negative pressure.
NPWT with intermittent suction has been shown to be of benefit for wound healing. This mode produces a mechanical stimulation of the wound bed (a massaging effect) and a greater circulatory stimuli, oxygenation and angiogenesis, and presumably a lower risk of occurrence of ischemic damage. Intermittent mode is however known to cause more pain.
New pressure cycles, without going to 0 mmHg suction, but only lowering the suction, to 50 % for example, should be able to maintain the highest degree of blood vessel 9
NPWT
formation and also a significant decrease in pain compared with the traditional intermittent group.
Under special wound conditions, when the wound involves structures such as the peritoneum, between toes, in tunneling injuries, in sternotomies, in the presence of high levels of exudate and when using NPWT on grafts or skin flaps, the continuous mode is the option of choice.
- Wound fillers
The choice of wound filler has been shown to have significant effect on wound healing. The commonly available material for this include foams and gauges with different pore sizes, stability etc.
The pressure distribution is similar for gauze and foam in dry wounds and the differences in performance are related to the structure of the material and its mechanical effects in the wound. The degrees of micro- and macrodeformation of the wound bed are similar after NPWT regardless of whether foam or gauze is used as wound filler. The increase in blood flow following NPWT is also similar with all wound fillers.
Wound contraction is more pronounced with foam than with gauze. Wound fluid retention is lower in foam, while more fluid is retained in the wound when using bacteria and fungus-binding mesh.
Thus NPWT may be tailored to the individual wound type to optimise the effects and minimize the complications by choosing different wound fillers. The choice of filler may be made with regard to the morphology of the wound, the wound characteristics, the patient feedback, possible infection and scar tissue formation.
o Wound morphology
Different wounds have different shapes and depths and thus require different fillers. 10
NPWT
Foam may fit better into a wound with a uniform shape, while gauze may be easier to apply in wounds that have an irregular shape, or with undermining edge since it can be better manipulated to the shape of the wounds. Different wound fillers can also be combined. Over a thin graft or a wound sleeve, the gauze will give a more appropriate cover. Foam may be advantageous for ‘bridging therapy’ since the foam compresses to a greater extent and thereby contracts the wound and speeds up the closure.
o Exuding wounds
In heavily exuding wounds, foam at a higher pressure (−120 mmHg) may be useful,
Since foam is less dense than gauze and a higher level of negative pressure drains the wound quicker.
o Wounds at risk of ischemia
In circumstances where there is a risk of ischemia, a lower pressure (−40 to −80 mmHg) and using gauze may be considered.
o Infected wounds
Various wound fillers designed for infected wounds include foam with silver, gauze that is impregnated with PHMB, gauze that is impregnated with silver, bacteria and fungus binding mesh.
Instillation techniques allow the irrigation of the wound with antiseptic solutions.
o Tendency to form excessive granulation tissue
Areas such as joints, where movement of the skin and the underlying tissue occur, may benefit from the use of gauze. Foam allows rapid growth of granulation tissue and may be a better choice in wounds where large amounts of granulation tissue is desirable, for example, postsurgical wounds such as sternotomy wounds.
- Wound contact layers
11
NPWT
Removal of foam used as fillers in NPWT can lead to pain and trauma. When the clinician anticipates such complications, a non- adherent wound contact layer such as paraffin or silicon may be placed over the wound bed beneath the wound filler. A wound contact layer also may be placed over vulnerable structures such as blood vessels or nerves. This wound contact layer may reduce the pain during dressing changes.
However keeping the quality of wound healing in mind, it is important to use wound contact layers only when there are structures to protect, in order not to slow healing.
- Protection of tissues and organs
NPWT can at times be the only option available to the treating clinician for managing highly infected and large wounds. However of late there have been reports of serious associated complications of NPWT.
The risk of right ventricular rupture and bypass graft bleeding following NPWT of mediastinitis is estimated to be between 4–7 % of all cases treated. Severe bleeding of large blood vessels such as the aorta has also been reported in several patients receiving NPWT. The incidence of NPWT-related bleeding in patients with exposed blood vessels or vascular grafts (such as femoral and femoral-popliteal grafts) in groin wounds were relevant in some studies. Severe bleeding has also been reported in patients receiving NPWT for burn wounds.
FDA has thus stated that NPWT is contraindicated in certain types of wounds: those with necrotic tissue with eschar, in non- enteric and unexplored fistulas, where malignancy is present, in wounds with exposed vasculature, anastomotic sites, exposed nerves, exposed organs and untreated osteomyelitis. 12
NPWT
It has been suggested that exposed sensitive structures need to be protected either through the interposition of autologous tissue (muscle flaps) or with heterologous material (dermal substitutes) or a number of wound contact layers.
- Pain treatment
Pain is a significant issue associated with NPWT and may affect patient adherence.
In patients that are neuropathic or paraplegic, where the pain is not of a significant nature, the filler can be used efficiently. In patients with low adherence, especially children and the elderly, and on painful lesions (such as pyoderma gangrenosum, burns, PUs and infected wounds), gauze, tends to be better tolerated.
Another option to reduce pain due to NPWT is to prepare the patient by infiltration of the wound filler with saline solution or local anaesthetics before dressing change.
Clinical Applications5
- Acute wounds
Acute wounds are often traumatic but can also be due to surgical debridement of infected or necrotic tissue. Wounds requiring extensive surgical debridement often present a wound dressing challenge due to anatomic location (eg, Fournier's gangrene), the size of the tissue defect, or the patient's body habitus.
- NPWT dressings can be applied immediately following operative debridement, which simplifies postoperative wound care. The ability of the foam and adhesive dressing to conform to almost any wound contour, shape, or size contributes to the success of NPWT in these complex wounds.
- NPWT can also be used in conjunction with skin grafts or flaps, which are frequently needed to cover tissue defects. NPWT has been used instead of traditional bolstering methods to provide skin graft fixation. The NPWT dressing distributes negative pressure
13
NPWT
uniformly over the surface of the fresh graft, immobilizing the graft with less chance of shearing leading to improved qualitative skin graft take and quantitative improvements in skin graft success.
- For acute open wounds, NPWT is associated with a reduced time to wound closure. NPWT has also been used to manage acute wounds resulting from lower extremity fasciotomy, degloving injury, open amputation, and complex traumatic wounds with exposed tendon, bone, or orthopedic hardware.
- NPWT may also have a particular role in the treatment of burn wounds.
- Chronic wounds
- NPWT may improve the healing of some types of chronic wounds/ulceration, such as diabetic foot ulcers, pressure ulcers, and open abdomen, provided that the wounds are well vascularized
- Post-sternotomy mediastinitis is an uncommon but devastating complication of cardiac surgery which may require the use of NPWT to manage the open wound while awaiting sternal closure.
- Prophylactic use
Evidence suggests that there may be a prophylactic role for NPWT in reducing the rates of surgical site infections.
Indications of NPWT
Trauma & Orthopedic Surgery
- Acute trauma & dermatofasciotomy wounds
NPWT is a tool in the treatment of traumatic wounds and high-risk incisions after surgery in
- contaminated acute wounds (open fractures, penetrating injuries) and wounds with tissue defects requiring a step wise procedure.
14
NPWT
- amputation stump resulting from a guillotine-like marginal zone amputation.
- management of motorcycle spoke heel injury
- perineal trauma-related wounds.
- Periprosthetic infections of the hip and knee joint
NPWT is a useful option in the management of early or delayed infections following implantation of an endoprosthesis.
- Osteomyelitis and surgical site infection
- Exposed tendon, bone and hardware
NPWT is the treatment of choice in such conditions where plastic surgery procedures cannot be used to provide immediate cover to exposed structures.
Acute burns and scalds
The management of burns with their associated high-fluid exudate following burn excision and skin grafting has always posed a challenge in burn wound care. The ideal dressing should protect the wound from physical damage and microorganisms; be comfortable and durable; allow high humidity at the wound; and be able to allow maximal activity for wound healing without retarding or inhibiting any stage of the process. NPWT fulfils all these criteria.
Plastic and reconstructive surgery
NPWT has produced a change of paradigms within the treatment algorithms in traditional reconstructive surgery.
NPWT may represent a valid alternative to immediate reconstruction in selected cases of acute complex traumas of the lower limb.
NPWT is a valid tool for reliable fixation of skin substitutes, such as tissue-engineered skin substitute and split skin grafts in all severe traumatised wounds and is associated with improved graft survival. 15
NPWT
Abdominal Surgery
NPWT is one of the techniques used for temporary abdominal closure (TAC) in laparotomies with packing, ACS or severe septic intra-abdominal complications.
Cardiovacscular Surgery
While NPWT is the method of choice for management of poststernotomy mediastinitis, its use is also being advocated over closed sternal incisions to reduce the incidence of deep sternal wound infection.
Vascular surgery
- Infected blood vessels and vascular grafts
For high-risk surgical patients with a fully exposed infected prosthetic vascular graft, NPWT along with aggressive debridement and antibiotic therapy is an effective alternative to current management strategies.
- Lymphocutaneous fistulas
NPWT can be used for the management of lymphocutaneous fistulae resulting from axillary and inguinal lymph node dissections as well as surgery of the infra-inguinal vessels.
Non-healing wounds
- Leg ulcers
Although NPWT has been used extensively in non healing leg ulcers, there is limited rigorous RCT evidence available concerning the clinical effectiveness of NPWT in the treatment of leg ulcers.
- Pressure ulcers
NPWT is increasingly being used to manage PUs, most likely due to its flexibility, which allows the caregivers to insert it into a more complex and articulated therapeutic strategy.
- Diabetic foot ulcer
16
NPWT
The rationale for adopting NPWT in DFUs is related to its capacity of removing exudate, protecting the wound from exposure to the environment, reducing odor and helping debridement.
Complications of NPWT5
NPWT is generally safe and well tolerated. Some of the important complications include bleeding, infection, pain, organ damage, and possibly death. Such complications are most likely to occur when NPWT is applied to patients whose wounds have devitalized tissue or exposed vital structures (eg, organs, blood vessels, vascular grafts).
- Bleeding
Bleeding is the most serious complication of NPWT and can occur in hospitals, long-term care facilities, and at home. Minor bleeding during dressing changes due to granulation tissue at the base of the wound is common and is best managed with firm pressure to the wound surface.
Severe hemorrhage can occur during removal of foam that has become adherent to the granulation tissue below, especially in patients who are anticoagulated, or in patients with exposed vessels or vascular grafts. In patients with severe bleeding, direct pressure should be applied and emergency services contacted. Surgery may be needed to control bleeding.
- Infection
Infection related to the use of NPWT is often due to prior wound infection that was inadequately controlled prior to initiating NPWT. When infection is suspected the NPWT dressing in discontinued, the wound irrigated and debrided, wound cultures obtained, and empiric antibiotics initiated.
- Enterocutaneous fistula
17
NPWT
Contraindications of NPWT21
- Risk of bleeding
NPWT should not be applied in wounds with manifest bleeding or a risk of bleeding, as suction could result in a significant blood loss.
Additionally the bleeding can clot the foam and therefore stop any function of the NPWT device.
- Exposed vessels and vascular prostheses
FDA has stated this as one of the contraindications for the use of NPWT.
- Necrotic wound bed
Necrotic tissue acts as a barrier to new tissue growth. The use of NPWT must therefore be preceded by radical debridement.
- Untreated osteomyelitis
Due to the deep extension of a potential osteomyelitic focus, simple surface treatment is unlikely to be successful. In this case, treatment must include the radical removal of the focus of infection.
- Malignant wounds
NPWT is known to promote granulation tissue growth and is therefore used for the purpose of improving tissue perfusion and enhancing granulation tissue formation. As a consequence, it should not be used in the presence of malignant neoplastic tissue.
NPWT can be useful as a purely palliative measure in inoperable cases. When used as a purely palliative measure, it allows wounds to be covered in a hygienic and clean manner.
NPWT is known to promote granulation tissue growth and is therefore used for the purpose of improving tissue perfusion and enhancing granulation tissue formation. As a consequence, it should not be used in the presence of malignant neoplastic tissue.
NPWT can be useful as a purely palliative measure in inoperable cases. When used as a purely palliative measure, it allows wounds to be covered in a hygienic and clean manner.