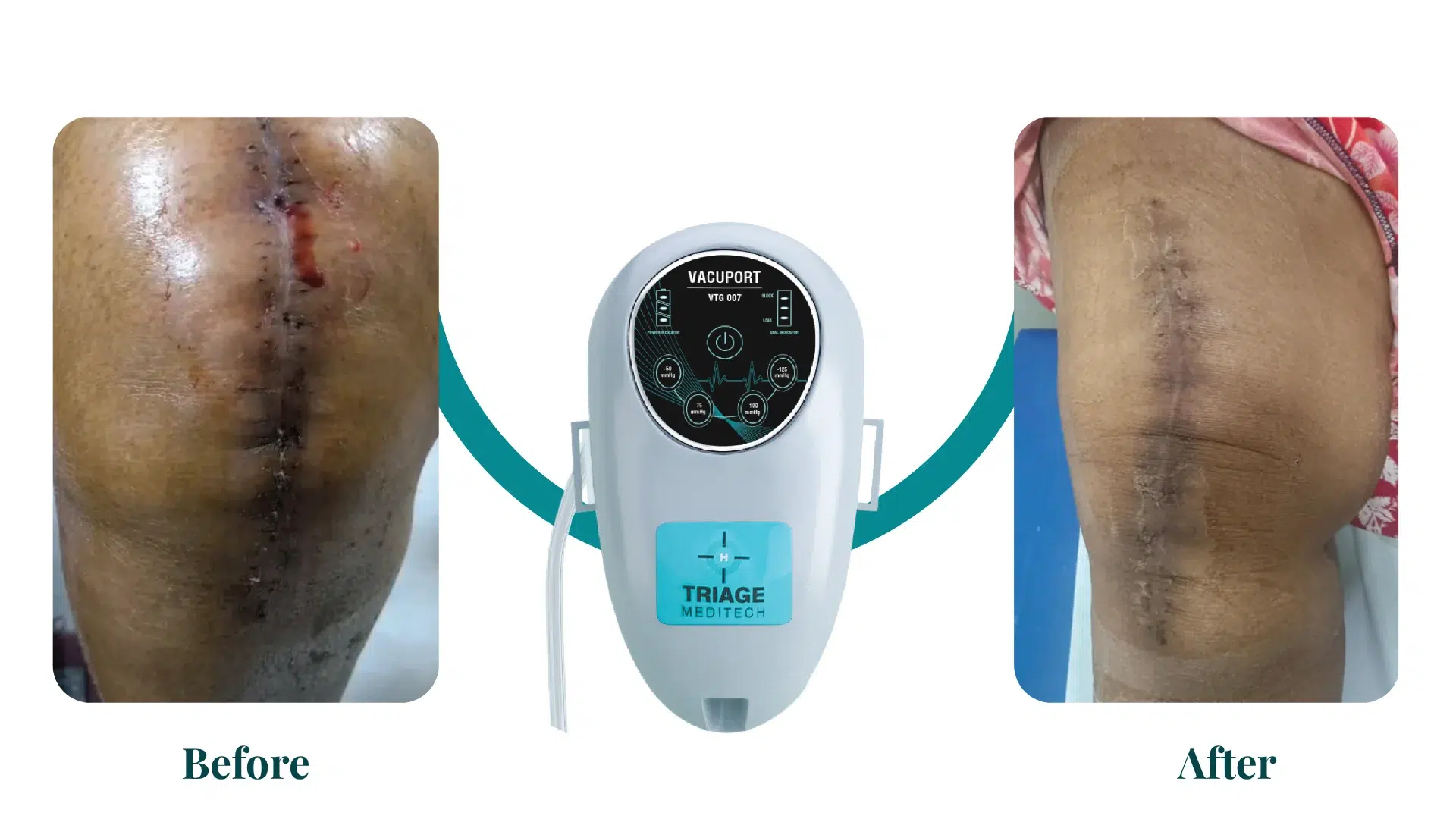
The science behind VACUPORT Incision Management is a specific application of a broader medical technology known as Incisional Negative Pressure Wound Therapy (iNPWT). It’s not just a dressing; it’s an active, biomechanical process that manipulates the wound environment to promote healing.
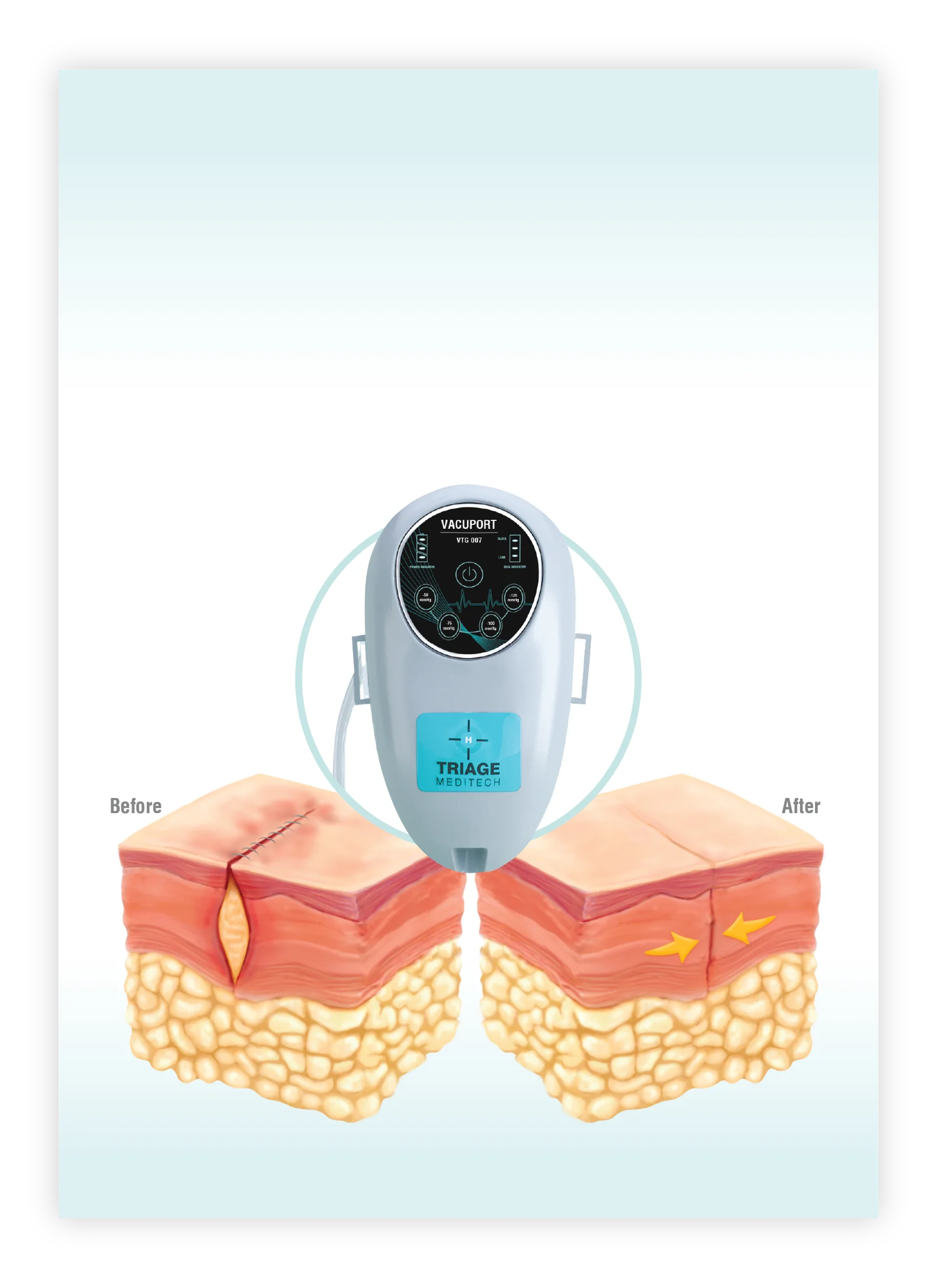
Macro- and Micro-Deformation
Macro-Deformation: The continuous negative pressure (-125 mmHg) delivered by the Vacuport system causes the foam dressing to compress and collapse. Because the dressing is sealed over the incision, this collapse applies an inward force, which helps to pull and hold the edges of the surgically closed wound together. This relieves tension on the sutures or staples and creates a more stable environment for healing.
Micro-Deformation: At a microscopic level, the negative pressure also causes a subtle mechanical stretching of the cells in the tissue beneath the dressing. This micro-stretching is a powerful stimulus for a process called mechano-transduction. It signals the cells to proliferate and migrate, which are essential steps in the formation of new tissue (granulation tissue) and the overall healing process.
Fluid and Exudate Management
Removal of Excess Fluid: A key function of the negative pressure is to actively remove fluids (exudate) and other materials from the wound site. This reduces swelling (edema), which can compress blood vessels and impair blood flow.
Reduced Bacterial Load: By constantly removing fluid, the system also flushes away a significant portion of bacteria and other contaminants that can lead to infection. A moist but not saturated wound environment is ideal for healing, and the Vacuport system helps maintain this balance.
Increased Perfusion and Oxygenation
While the pressure might seem like it would restrict blood flow, studies have shown that NPWT actually increases perfusion (blood flow) to the surrounding tissues. The removal of edema and the mechanical stimulus from the negative pressure can help open up the micro-vasculature, bringing more oxygen and nutrients to the site and removing waste products. This improved blood flow is a critical factor in accelerating the healing process.
Creation of a Closed, Protected Environment
The sealed dressing creates an airtight barrier that protects the surgical incision from external contamination. This is especially important in a hospital setting or for at-home use, where there is a risk of exposure to bacteria and other pathogens that could lead to a surgical site infection (SSI).
The dressing also contains a skin interface layer that often includes ionic silver, which helps to reduce bacterial colonization within the fabric itself.
In essence, Vacuport takes the principles of Negative Pressure Wound Therapy and applies them to a closed incision, turning a passive dressing into an active, protective, and therapeutic device. It helps the body’s natural healing processes by controlling the physical and biological environment of the wound to reduce the risk of complications and promote faster, more robust healing.